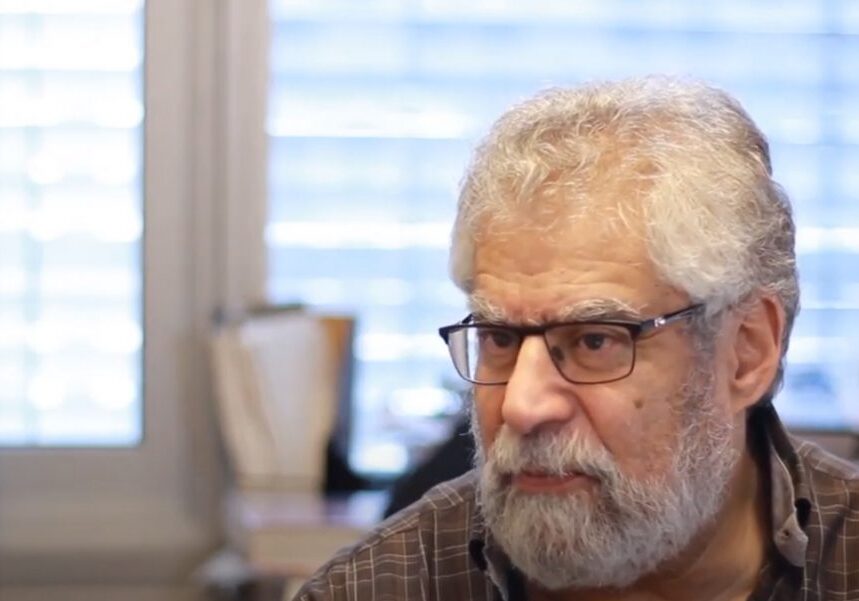
Michael Sefton
University Professor & Michael E. Charles Professor
PEng
Research Stream: Cell & Tissue Engineering
Email & Telephone: directory.utoronto.ca | Office: Donnelly Centre, 160 College Street, Room 406
Main Appointments
- Department of Chemical Engineering & Applied Chemistry
- Institute of Biomedical Engineering
- Executive Director, Medicine by Design
Additional Appointments
- Terrence Donnelly Centre for Cellular & Biomolecular Research
Research Interests
Cell Transplantation / Drug Delivery
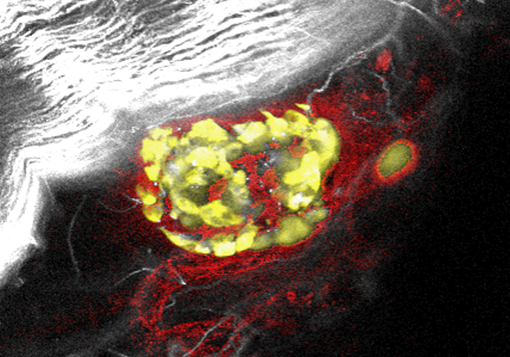
Mammalian cells may be microencapsulated within a biocompatible polymer membrane in order to facilitate their transplantation. The polymer, being permeable to glucose and other nutrients, allows the cells to remain viable and function normally (e.g., secrete a hormone). However, the membrane is impermeable to the higher molecular weight antibodies so that the cells are not rejected when implanted. Preserving the cells’ viability during encapsulation (e.g., during exposure to organic solvents) is extremely difficult and we appear to be the only group in the world that can do this with a biocompatible polymer. Our polymer (poly HEMA-MMA) is very similar to soft contact lens material. We are involved in making better polymers, designing more efficient processes for making capsules or understanding what happens to the cells, in vitro or in vivo, when they are enclosed inside the capsule. Current applications include the encapsulation of pancreatic islets for the treatment of diabetes, dopamine producing cells for the treatment of Parkinson’s disease or the use of genetically modified cells for gene therapy. The Sefton lab is particularly interested in modulating the immune and inflammatory response using genetically modified cells to these capsules upon implantation.
Biomaterials
The Sefton lab are also investigating blood compatible materials. Blood clots when it comes into contact with synthetic materials. Hence in the preparation of devices that are used in contact with blood (e.g., artificial heart, vascular grafts, catheters), techniques must be used to disperse clots or prevent their formation. The administration of anticoagulants (heparin) is commonly used to prevent the blood from clotting (however their use may lead to excessive bleeding). In the past our approach was to covalently immobilize heparin onto the material surface, through a polyvinyl alcohol (PVA) coating layer. This has been very effective in preventing adherent clots but embolization and the consumption of platelets continues to be a problem. Hence we have focused on understanding why PVA is reactive and on developing alternatives to PVA that can be heparinized yet are not so reactive. Flow cytometry and other immunologically based techniques are fundamental to these studies. We are also interested in the links among coagulation, platelet and leukocyte activation and complement activation. This and our interest in cell encapsulation has lead us to investigate the mechanism of biomaterial associated inflammation.
Tissue Engineering
These projects relate to the University of Toronto initiative in Tissue Engineering which is described more fully elsewhere. Although these problems have a significant biomedical orientation (making them suitable as thesis projects for non-engineering students), the difficulties that arise generally necessitate the use of well established engineering approaches. Hence a student in this area will have the background to handle difficult problems not only in biomedical engineering but in other areas also.
News & Stories
Current students registered with BME
No users found.
Alumni graduate with BME degree
15 users